An interview with MDGuidelines, an online platform for medical disability durations and the American College of Occupational and Environmental (ACOEM) clinical guidelines on occupational health, case management, and disability duration guidelines.
In today’s fast-paced business landscape, organizations with occupational health (OH) clinics understand the importance of efficient case management. Ensuring employees’ well-being with the right treatment at the right time coincides with minimizing operational disruptions and financial impacts.
Case management is a complex process that requires coordination, communication, and collaboration among various stakeholders. The goal is to facilitate timely and effective return to work (RTW), reduce disability costs, and improve employee satisfaction and productivity.
However, case management is not a one-size-fits-all solution. Each case is unique and requires a customized approach based on the best available evidence and the specific needs and preferences of the worker and the employer.
Julianna Giordanella, Product Marketing Manager at Cority recently sat down with Kerri Wizner, MPH, an occupational epidemiologist at MDGuidelines, to discuss evidence-based guidelines within case management.
In this interview, we discuss:
- Ways OH teams and case managers can remain up-to-date and aligned with the latest medical research and industry best practices
- Emerging occupational health and safety challenges that companies should be preparing for
- Why having an integrated OH and duration guidelines solution is necessary to meet mandatory reporting timelines
- Advice to Occupational Health professionals for providing optimal employee care while addressing clinical and financial challenges
Julianna Giordanella (JG): Why are early intervention opportunities within case management so important?
Kerri Wizner (KW): Early intervention is important to proactively address health issues and prevent unnecessary departure from peoples’ normal, active lives due to illness, injury, or chronic conditions.
From research, we’ve found setting expectations at the point-of-care significantly helps outcomes. Proactively discussing questions can be helpful, such as, “What are the patients recovery goals” and “Are they prepared to discuss options for modified duty with their boss?”. For patients, knowing what’s going to happen on the pathway to recovery is valuable for managing stress and the unknown, related to the disability process.
A study in the journal Surgery found that setting pain expectations before a procedure can reduce the number of opioids people ask for afterwards, because patients are ready to manage some pain during recovery.
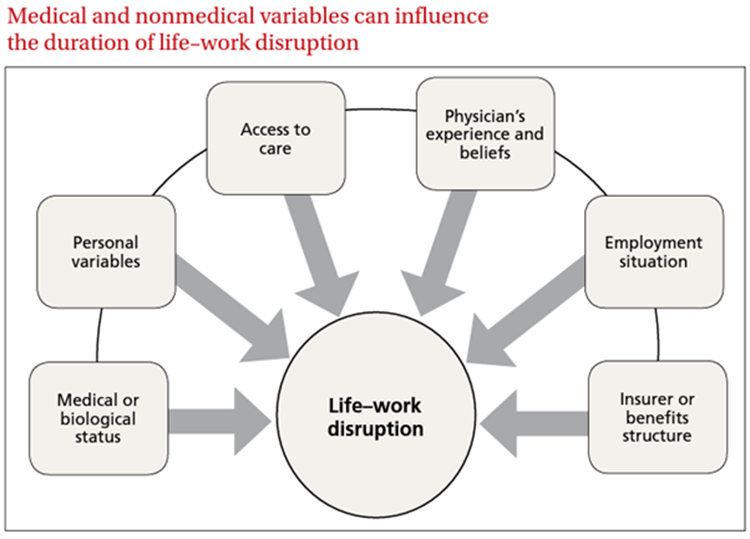
Figure 1. Managing work disability to help patients return to the job involves many stakeholders. Case managers are often in the best position to advise next steps to recovery.
When patients have multiple touch points with case management professionals that can access real-time, evidence-based information, it can really make an impact by establishing the evidence-based expected next steps.
Think about all of the medical and nonmedical variables that influence the duration of life-work disruption. Case managers are generally the only people that are reaching into each of these buckets to help patients. Therefore, using evidence-based guidelines to assist these different conversations can help quickly narrow down topics that are most relevant to the patient and their diagnosis. This also can help advise the patient on how to advocate for themselves, which is especially important when they talk to their employer about stay-at-work or return to work (RTW) options, which is really unique to case management.
JG: Can you share some emerging challenges companies and OH teams are focusing on and why?
KW: The biggest challenge I am hearing about is how to deal with mental health conditions.
Many companies are taking positive steps by offering preventative support such as fostering healthy work environments and encouraging well-being, but in many cases, this is not enough. The COVID-19 pandemic was a hard time in people’s lives and we’ve seen mental health cases steadily increase in its aftermath.
Once someone is diagnosed with a mental health disease, it seems like the people around them, including employers, freeze and don’t know what to do next. Additionally, while mental health can be tricky, we should be treating it the same as physical injuries – Look up the expected outcome, have open dialogs about RTW expectations, and get creative with stay-at-work or modified duty programs.
One area of research we’re expanding on is cognitive demand.
In the past for short-term disability, we’ve mostly focused on the physical demands (such as if a person can pick up a 20-pound box) to determine how long they are out, but this isn’t necessarily applicable for mental health conditions. Occupational health specialists should also consider the cognitive, psychomotor, and sensory abilities that are needed to be successful at work. The industry hasn’t really picked up on that yet and I think it is worth exploring.
JG: What types of organizations or industries can benefit the most from assessing disability duration guidelines into their case management processes?
KW: We should be thinking in broader terms – beyond industry divisions, and even beyond working with disability clients. As patients in the medical system, every person should be getting evidence-based care. We have an opportunity in disability management to meddle a bit and help ask the right questions, so people get the best care and return to their normal lives quickly and safely. With the standard 8-minute medical appointment, it is hard for medicine to do everything, and case management has the chance to help working-aged people have the best experience possible when they’re sick or injured.
Setting disability duration guidelines as the gold standard for workers compensation care helps on many levels including overall reporting and preventative care and therefore should be applied across a broad range of companies.
JG: Can you share some benefits of having an integrated OH and duration guidelines solution OH professionals can access?
KW: Having an integrated occupational health system is key! Integrating guidelines into the system and leveraging them at the point-of-care can enable better case management and decision-making, which can lead to faster recovery times and lower costs. It helps to save time down the road, especially when a case manager or clinician has access to all relevant data. Our research is constantly being updated – there are more than 1,200 topics people can access and benchmark.
For example, case managers could use the integration to compare how long the injured person has been out of work versus the expected duration, and review if rehabilitation is right on target or way beyond where progress should be.
Another example is caseload assistance. I’ve seen case managers using dozens of internet tabs because they have to reference many different sources of information. Integrating a case management tool with evidence-based guidelines helps everyone use their time more efficiently and ensures access to trustworthy information, almost like a short-cut for experience. The information, the data, the research, patient history, industry benchmarks, it’s all in one place.
In this instance, integrated case management is empowering case managers to restore employees’ health and help them RTW by coordinating care in the most efficient and cost-effective way.
JG: How can OH teams and case managers stay up-to-date with medical research and best practices for disability duration guidelines?
KW: It’s tough out there.
I saw one statistic from Nature that found more than 1 million biomedical peer-reviewed journal articles are published every year…that is about 2 papers per minute, and that number is growing by 5-10% per year. That volume makes it nearly impossible for case managers or clinicians to keep up with the latest research recommendations. Additionally, it’s not just reading the articles, but also the time it takes to determine how the research affects their cases or patients.
Good guidelines take time to make. It requires a review of all the available research, a synthesis of that research, and then review by a variety of experts about the conclusions.
And so, I think where case management leadership comes in is actively applying guidelines. Making sure that there is institutional support to reference those guidelines, by making them available and giving case managers the time to look up guidelines, which requires some kind of top-down policy.
I know that continuing education credits and professional conferences are great ways to engage people and keep them interested, but again they require leadership support to allow people to attend learning sessions.
MDGuidelines and ACOEM offer a number of webinars and research briefs each year on a variety of topics to help showcase new and interesting trends in evidence-based medicine. For example, our latest research brief highlights best-practice guidance for opioids.
JG: Millions of workers leave their jobs each year due to health-related reasons. Is there any advice you’d give health professionals to help them address the challenge of achieving optimal clinical and financial outcomes while ensuring better employee care?
KW: My advice would be to use data to make good decisions and be creative. A lot of research has found that stay-at-work options and an empathetic employer can go a long way. Review your claims data from past years, find a condition where you have a lot of variation in RTW and devise an intervention to help everyone with that condition return to work a little bit sooner. You’d be surprised what you can find in the data.
JG: What are some examples or measurable outcomes from organizations that have adopted disability guidelines?
KW: Earlier, I mentioned that it is important to review previous years’ claims and see where an organization or client could do better.
Here at MDGuidelines, we offer benchmarks to review claims. For example, for any diagnosis, let’s say depression, we can see how the claims look compared to population-level benchmarks and physiological optimum. If there is a big difference between population-level estimates and a company’s own data, that is to say that their own people are returning to work later than population estimates, that is an opportunity for focused case management. This is because we know that, on average, people can RTW sooner, but the company’s claims are not reflecting that, so there is something likely occurring that is not health related.
Furthermore, with the integration into a larger Occupational Health solution to manage cases, you get the benefit of having estimates all in one unified platform and you’re able to see and report on it more easily. Another benefit is that the frontline case managers have access to all the necessary information in one place and will be able to make changes in real-time.
Cority and MDGuidelines share a vision of empowering case managers to deliver the best possible care and services to employees.
By providing necessary resources, organizations can improve quality of care, reduce the time spent away from work, and save money.
That’s where Cority and MDGuidelines come into play, offering seamless occupational health and safety software solutions for organizations looking to optimize their case management processes. The value is not just the data, but how to use the data and apply it in real life. Empowering organizations by enhancing the capabilities of their internal occupational health clinics, improving employee well-being, and streamlining the return-to-work process.